Non-Epileptic Seizures
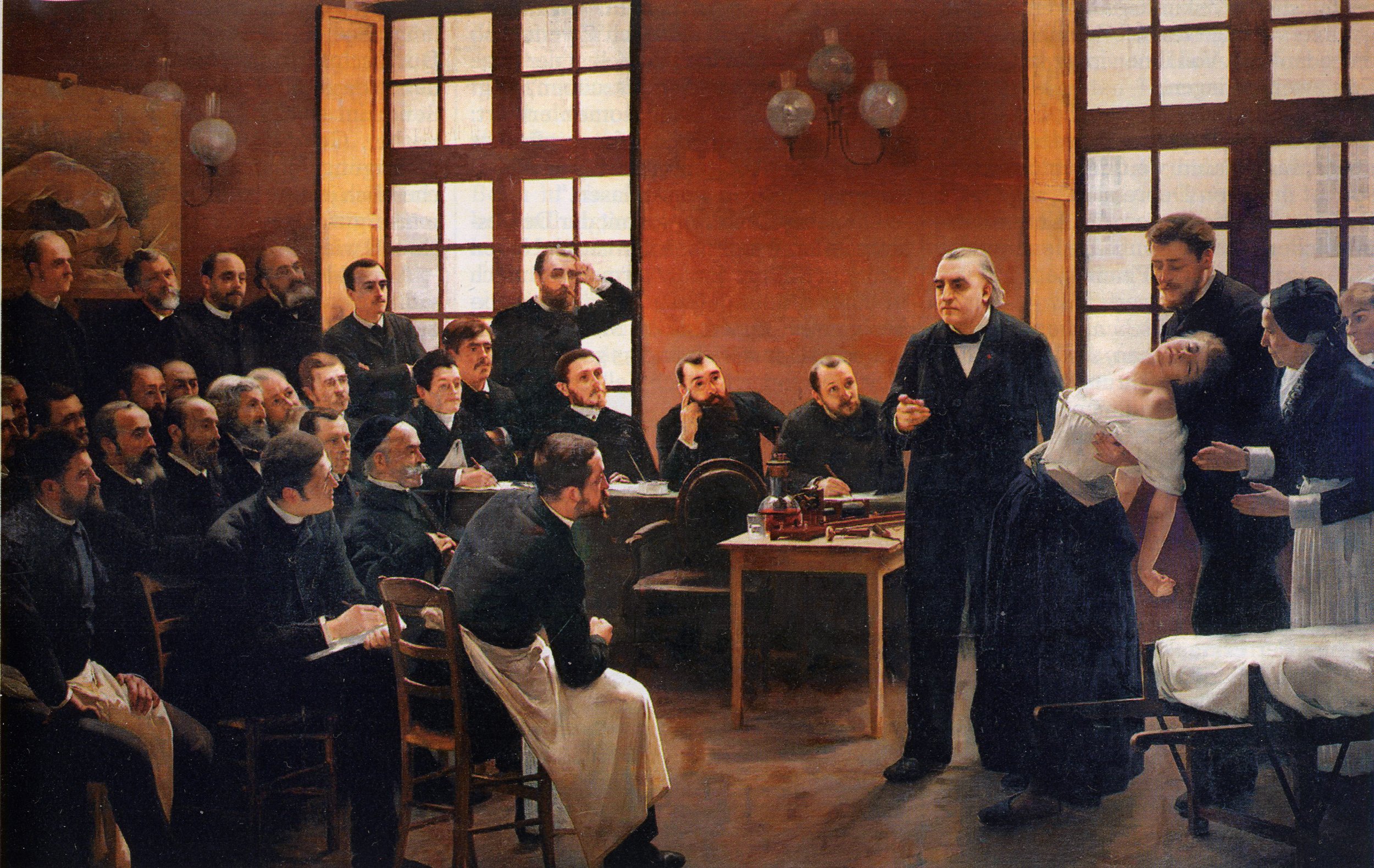
The father of modern neurology was Jean-Martin Charcot. While many remember him for his work in neurophysiology and neurobiology, it is arguable that the majority of his work was identifying symptoms and syndromes that would later be called Conversion disorders, now termed Functional Neurologic Disorders (or FND). It was such a key part of his research that the most famous image of him was teaching other neurologists about patients with seizure-like episodes that could be cured through hypnosis. If you look closely, you can see his patient in an identical posture to the painting in the back of the room, a visual representation of how classic the syndrome was and how it could be identified positively due to those features.
Une leçon clinique à la Salpêtrière
Dr. Charcot teaching his students (now very famous neurologists) about the treatment of a non-epileptic seizure patient in the late 1800s
Another fact about Dr. Charcot that people often neglect is that he was alive before the great schism between neurology and psychiatry. At the time, nearly everyone studied both, and they were seen as inseparable for a proper training in the diagnosis and treatment of the disorders of the nervous system. Just as Dr. Babinski was a student of Dr. Charcot, so was Dr. Sigmund Freud. This relationship was so strong, that Sigmund Freud named his first son Jean Martin. It could even be argued that Charcot was a bigger advocate for the use of hypnosis than Freud who found that the results were powerful, but ultimately transient with symptoms returning within hours to days after the procedure.
What made the diagnosis easy to identify? Simply this, there are many things that the body cannot do when it is having seizure activity in both halves of the brain. If someone is having an epileptic convulsion, they cannot be awake through the seizure. They cannot hold certain postures and positions. They cannot respond to certain exam techniques in certain ways. There are also some inaccurate “rules” that are taught to medical students about non-epileptic seizures. It was previously taught that a non-epileptic seizure shouldn’t result in injury, but this and a few other assumptions were never part of the early phenomenological descriptions, and I’ve never found data to support them. I’ve also seen in practice that they are untrue. Nevertheless, most neurologists rely on hard signs that always help to differentiate these two types of seizures.
As the decades moved on, the psychiatrists and psychologists continued to have the most effective treatments for these patients who convulsed without aberrant electrical activity in the brain that we call epilepsy. In the beginning, the theory was that deep psychological forces would convert to a physical symptom like the seizure. The goal of treatment was to identify the source of that psychological conflict and by treating it, reduce the seizures. As the field evolved from psychoanalysis, through behaviorism, into structured therapeutic modalities, the treatments for this conversion disorder adapted as well and each modality has included techniques to treat it.
Currently, the most well validated approaches include a mixture of psychotherapy and medications. Step one is to identify any comorbid psychiatric diagnoses such as PTSD or Major Depression and begin treatment for that condition. Then, in a series of sessions, the patient and therapist discuss the nature of the symptom, making sure the patient has a good understanding of the nature of it and the plan for treatment. This includes both medical education, such as why the convulsion is not epilepsy, about how the brain is creating the symptom, and that the psychological approach is a scientifically valid treatment. Then, a series of steps are taken to help the patient discover patterns of the symptom, what triggers the symptom, what events lead to those triggers, and how to intervene in those earliest stages to disrupt the cycle. A good approach will include some searching for deeper components, but this can often be done without naming any of the primary traumas or psychological underpinnings of the symptom.
Other techniques used to interrupt the cycle include skills under categories such as mindfulness exercises, distress tolerance, and emotional regulation. The simple act of recognizing the earliest sign that the FND symptoms will manifest, what triggers them, and introducing skills to abort the symptoms can be extremely effective and in many cases will completely resolve the FND syndrome. It is very difficult work, much harder than taking a pill to reduce epileptic seizures. However, the skills used in treatment can have a meaningful long term impact on overall health measures. The same skills can help someone change their habits to prevent heart disease, treat insomnia, and simply function better in their day to day lives.
If you would like to discuss your non-epileptic seizures, understand more about what other disorders could play a role in your symptoms, and consider what treatment modalities are right for you, contact us for a consultation today.